Understanding Health in the Big Picture
By Jill Van Den Bos, Shelley Moss and Stoddard Davenport
Health Watch, August 2021

Social determinants of health (SDOH) have been a topic of growing interest in recent years, yet consensus about what the phrase represents and how health-related social needs should be studied or addressed by employers, health plans, providers and other stakeholders in the business of health care has been lacking. For many, low-income populations come to mind when considering the topic, yet SDOH include a wide range of factors beyond income. Many types of data are available, yet each presents distinct challenges and opportunities for analysis. In this article, we describe some of the underlying context for considering SDOH, as well as some of the potential data sources to consult and challenges to grapple with on this important topic.
Going Upstream
Imagine that you are fishing in a river with a group of friends, and you see someone in the water shouting for help. You go to rescue them, but soon you see more people in the water in need of help, and the situation is becoming overwhelming for your small group to solve. One idea is to triage and rescue those who are about to drown first. Another idea is to build a raft and coordinate a mass rescue. You can see the benefit to either of these ideas, but neither gives a complete solution to the problem. People in need of rescue continue to float down the river. Then it dawns on you—you need to go far upstream to find who or what is throwing these people into the water. This story is the often-repeated public health parable called “The Upstream Story.”
Drawing the analogy to health care, the first idea of triaging rescue for those in most dire need is represented by emergency department (ED) doctors, intensive care unit (ICU) specialists and others who help those in acute crisis. The second idea of coordinating a mass rescue is represented by primary care physicians and others who provide traditional preventive care and care management for chronic conditions. While these clinicians provide valuable and even life-saving services, the health care system needs upstream providers. Health and wellness and, on the flip side, illness and risk factors originate far upstream: not in clinics and hospitals, but in our homes, neighborhoods and communities. To address the health of the populations they serve, health systems would do well to understand the wider social needs and provide services outside of “traditional” health care.[1]
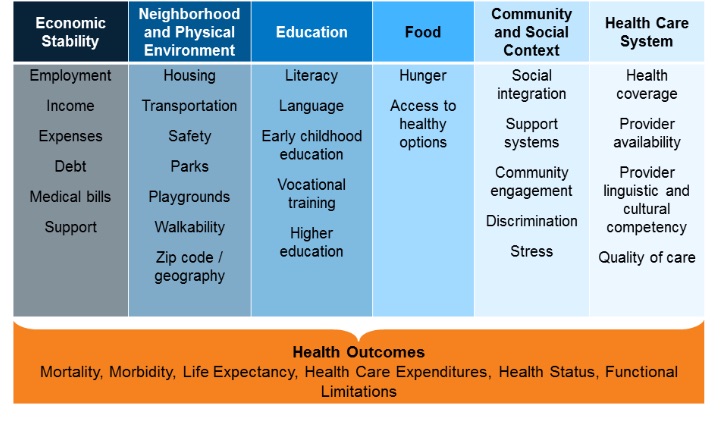
The observation that your zip code is a better predictor of your health than your genetic code is a well-known yet nevertheless startling thought.[2] Also eye-opening is that SDOH may account for as much as 50 percent of the modifiable contributors to health outcomes.[3] The U.S. Department of Health and Human Services (HHS), in its introduction to Healthy People 2030, describes SDOH as "the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks."[4] These conditions include socioeconomic status, education, neighborhood and physical environment, employment, social support networks and access to health care.[5]
Figure 1 presents a graphic from the Kaiser Family Foundation that illustrates items that impact health outcomes.[6]
Figure 1
Social Determinants of Health
Source: KFF, https://www.kff.org/wp-content/uploads/2018/05/8802-Figure-1.png.
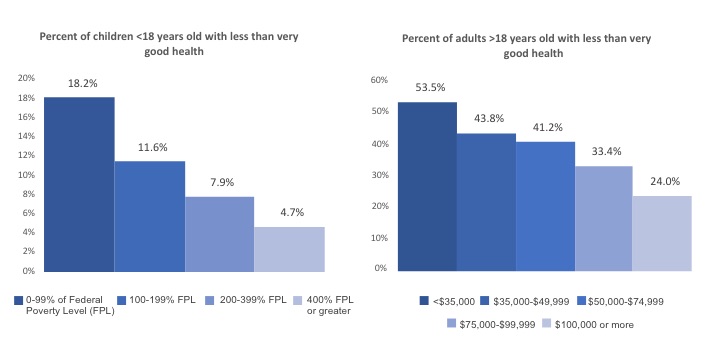
Health plan actuaries tend to focus on the elements in the column farthest to the right in this figure. However, the other features shown have material impact on health outcomes. Figure 2 presents the relationship between family income and health status for children and adults to illustrate the impact of just one of these features.
Figure 2
Health Status by Family Income Level, Children and Adults[7]
To the extent that SDOH have such impact on health and health outcomes, it is short-sighted for health plans and their actuaries not to investigate, understand, measure and use that information whenever possible. However, where can SDOH information be obtained?
Data Sources and Research Questions: Challenges and Opportunities
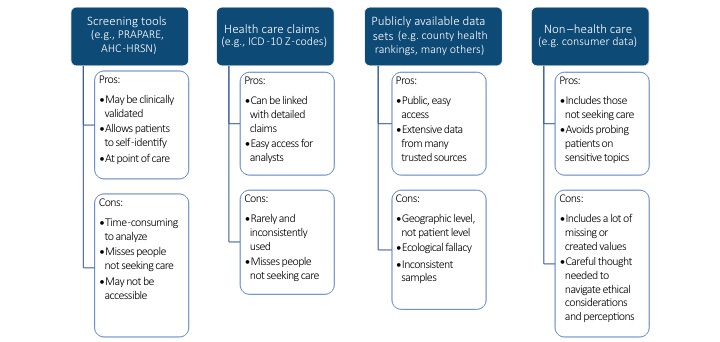
There are several potential sources of SDOH data, as shown in Figure 3.
Figure 3
Potential Sources of SDOH Data[8]
Note: PRAPARE = Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences; AHC-HRSN = Accountable Health Communities Health-Related Social Needs screening tool; ICD-10 = International Classification of Diseases, 10th revision.
None of the listed data sources is perfect. Health plans and self-funded employers/plan sponsors may be interested in using SDOH for various purposes, including identifying high-risk populations and individual patients appropriate for intensive intervention and informing administrative planning decisions related to targeted outreach, delivery system design, performance assessment (e.g., disparities analysis), and resource allocation (e.g., staffing and community investment). In addition to actuaries and health carriers, SDOH-enhanced predictive risk models are useful to other entities seeking to leverage such data to better serve patients with health-related social needs. These entities include other safety net providers; disparity researchers; health plans; employers; and federal, state and local governments.
A key question for actuaries is: how well do the various SDOH data sources perform for different analytical purposes? Understanding how to balance performance with the ease or difficulty of obtaining usable SDOH data could be helpful for users.
One study sponsored by the Society of Actuaries (SOA) used the first three data sources shown in Figure 3, plus electronic health record (EHR) data, to study SDOH in a Medicaid population.[9] The overarching goal of the study was to investigate how well easily accessible public health data compared to more informationally rich data from SDOH screening tools in predicting selected health outcomes at the individual patient level. Specific topics included the correlation between public health data and data from SDOH screening tools, how well SDOH data from the two sources predicted selected clinical outcomes, and how SDOH variables from the two sources contributed to patient risk classification.
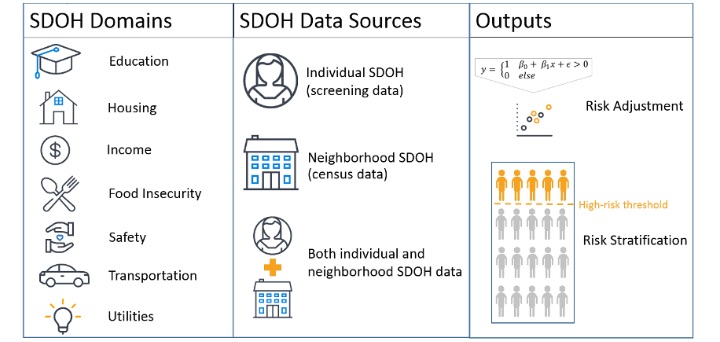
Figure 4 shows a simplified logic model that highlights key features of the project.
Figure 4
SOA Research Project Logic Model[10]
The first takeaway from the SOA study is that census-based neighborhood SDOH measures are not highly correlated to individual SDOH measures from screening data. It is therefore interesting that the second takeaway is that SDOH measures from either source provide modest predictive power for selected health outcome measures, yet using SDOH variables from the two sources together doesn’t provide much additional benefit. A third takeaway is that SDOH variables from the two sources identify different, albeit overlapping, groups of patients as being high risk for selected conditions. Many other conclusions might be reached from this research, but one significant observation is that success with research on SDOH topics requires a thoughtful effort to identify the right pairing of research questions and data sources. Not all potential research questions can be adequately addressed by commonly used data resources, but often a research question can be reframed in a way that can be addressed using available data while still providing meaningful insight.
It is important to note that SDOH measures are getting a lot of attention and are likely becoming better at representing data in a way that is more robust for research purposes. For example, researchers from the Center for Spatial Data Sciences at Searle Chemistry Laboratory have been studying the use of multidimensional instrumentation for creating measures of SDOH that represent multiple elements of social needs rather than a single index.[11] The availability of SDOH information for predictive analytics has never been better, although it still has room to improve.
SDOH information can be used to understand and predict member health and health risks, but more work is needed to determine how best to operationalize such efforts. Researchers have already given thought to this situation; for example, at the University of Maryland School of Medicine, work has been done on ways for payers and providers to partner to address SDOH.[12] Dr. Wayne Rawlins, who spoke at an American Academy of Actuaries webinar on health equity on May 24, 2021, noted that actuaries are in a position to identify and quantify the impact of SDOH and their impact on health (and health disparities). Some actuaries and health plans are looking at this information; it can be useful for adjusting out bias in predictive models, contributing to risk stratification for health care intervention and directly identifying the needs of members who would fall outside traditional health care services (potentially for community service referrals, for example). Perhaps it is time for more actuaries to lead their health plans upstream.
Statements of fact and opinions expressed herein are those of the individual authors and are not necessarily those of the Society of Actuaries, the newsletter editors, or the respective authors’ employers.
Jill Van Den Bos, ASA, MAAA, is a principal and consulting actuary with Milliman. She can be reached at jill.van.den.bos@milliman.com.
Shelley Moss, ASA, MAAA, is an associate actuary with Milliman. She can be reached at shelley.moss@milliman.com.
Stoddard Davenport, MPH, is a healthcare management consultant with Milliman. He can be reached at stoddard.davenport@milliman.com.
Endnotes
[1] Manchanda, R. What makes us get sick? Look upstream. (Video) TED. https://www.ted.com/talks/rishi_manchanda_what_makes_us_get_sick_look_upstream/transcript?language=en#t-468924 (accessed July 23, 2021).
[2] Roeder, Amy. 2014. Zip code better predictor of health than genetic code. Harvard T.H. Chan. https://www.hsph.harvard.edu/news/features/zip-code-better-predictor-of-health-than-genetic-code/ (accessed July 23, 2021.
[3] Park, H., A. M. Roubal, A. Jovaag, et al. 2015. Relative contributions of a set of health factors to selected health outcomes. Am J Prev Med 49, no. 6:961–969.
[4] U.S. Department of Health and Human Services. Social determinants of health. Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed July 23, 2021.
[5] World Health Organization. 2008. The World Health Report 2008—Primary Health Care Now More Than Ever. World Health Organization: iris. https://apps.who.int/iris/handle/10665/43949?search-result=true&query=The+World+Health+Report+2008%E2%80%94Primary+Health+Care+%28Now+More+Than+Ever%29&scope=&rpp=10&sort_by=score&order=desc (accessed July 23, 2021).
[6] Artiga, S., and E. Hinton. 2018. Beyond health care: The role of social determinants in promoting health and health equity. Kaiser Family Foundation. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ (accessed July 23, 2021).
[7] Data Resource Center for Child and Adolescent Health. National Survey of Child and Adolescent Health Measurement Initiative, 2018–2019 National Survey of Children’s Health (NSCH) data query. U.S. Department of Health and Human Services. http://www.childhealthdata.org (accessed July 23, 2021); Centers for Disease Control and Prevention. Summary Health Statistics: National Health Interview Survey, 2018: Table A-11a. Retrieved June 27, 2021, from https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-11.pdf (accessed July 23, 2021).
[8] National Association of Community Health Centers. PRAPARE: Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences. https://www.nachc.org/research-and-data/prapare/ (accessed July 23, 2021); Centers for Medicare and Medicaid Services. The Accountable Health Communities Health-Related Social Needs Screening Tool. https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf (accessed July 23, 2021); County Health Rankings and Roadmaps website at https://www.countyhealthrankings.org/.
[9] Everhart, R. M., J. Ven Den Bos, T. Gray, et al. 2020. Comparing Measures of Social Determinants of Health to Assess Population Risk. Society of Actuaries. https://www.soa.org/globalassets/assets/files/resources/research-report/2020/comparing-measures-social-determinants-report.pdf (accessed July 23, 2021).
[11] Kolak, J., J. Bhatt, Y. H. Park, et al. 2020. Quantification of neighborhood-level social determinants of health in the continental United States. JAMA Network Open 3, no. 1:e1919928, doi:10.1001;jamanetworkopen.2019.19928.
[12] Kannatkat, J. T., J. E. Hartle, and N. Parekh. 2021. Need for payer-provider partnerships in addressing social determinants of health. J Manag Care Spec Pharm 27, no. 6:791–796.